Public Value
Introduction
Healthcare organizations, whether concerned with finance, service provision or performance, require a mandate (mission statement) that defines their purpose and ensures their alignment with the other organizations within and outside the health system.
These mandates frequently require revision to ensure their currency with society needs and expectations. The strategic triangle, introduced by Moore, is a practical framework that can be used by decision-makers to review their organization mission and to ensure that it has appropriate support and there is capacity to deliver it.
Stratgeic Triangle
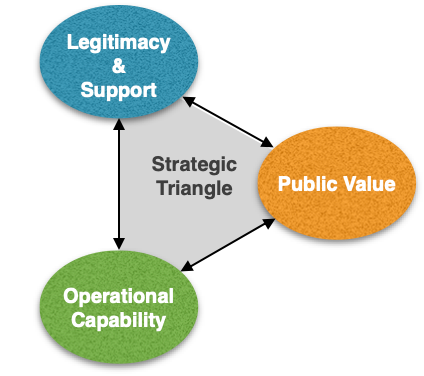
The strategic triangle is basically formed of three elements (see Figure). Firstly, decision-makers need to declare the organization’s mission (purpose) expressed in terms of the important public values it intends to deliver. Second, decision-makers are also requested to obtain legitimacy for their mission and ensure enough support will be available for its delivery and sustainability. Third, decision-makers have to ensure their operational capability in delivering the stated mission whether achieved independently or in partnership with other organizations.
Defining the public value that any organization intends to deliver is a challenge as it requires engagement with clients, through dialogue and deliberation at all levels, in order to truly understand what they value. However, decision-makers should also ensure that their organization not only satisfies their clients but also citizens at large by adding value to the public sphere through, for example, the creation of fair, inclusive and efficient organizations that are capable of sustaining public value over time.
In obtaining legitimacy and support for the defined public values (mission), decision-makers have to engage all those who can hold them to account. This engagement should be uninterrupted and sensitive to changes within the authorizing environment to ensure continuous support and adequate resources. Besides the law and political consent, authorizing environments include the public, the affected stakeholders, current knowledge, and community morals.
Operational capability includes the people, money, skills, space, knowledge, infrastructure, and specific resources needed to deliver the organization’s mission. Naturally, decision-makers should work towards making these capabilities available but not all these capabilities need to be present within a single organization. This is why it is important for healthcare organizations to have the capability of collaborating with other organizations in creating public value that clients and citizens expect. Furthermore, clients and citizens are considered nowadays coproducers in the creation of public value by pursuing behaviors that are not only conducive to maintaining their health but also to creating healthy environments in which to live.
The strategic triangle presents a simple and practical framework that decision-makers at all levels can utilize to ensure that their decisions and activities increase public value. It helps us to think outwards towards what we create and its relation to what the public wants. It directs us also to look upwards to ensure that we work within accepted boundaries and inwards to ensure that our capabilities fit with our intended work.
The strategic triangle can also be used as a public value scorecard with three perspectives for evaluating organizational performance as public value is not only achieved through outcomes but also through the processes that produce them.
Public Value Stream
Public value is usually created at the frontline of healthcare organizations where there is the most direct interaction between healthcare providers and patients, families and communities. Therefore, the adding of public value depends heavily on the competencies and commitment of frontline staff and is influenced by the organization’s governing policies, organizational culture, knowledge generation and communication within the organization, collaboration, education and training programs, and availability of adequate resources.
For example, healthcare providers cannot offer patients safe care with a minimum of adverse events except within a safety culture that has been developed across the organization. This safety culture requires staff who have been trained to learn from their mistakes and take proactive measures to minimize future risks with the active participation of patients and their families.
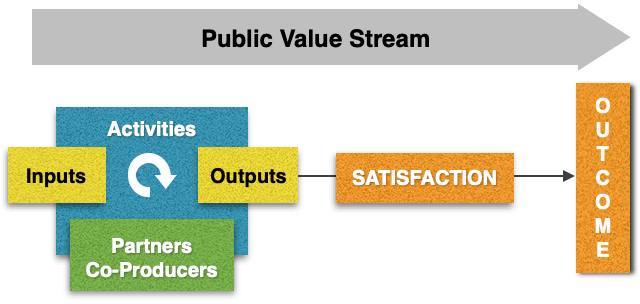
The public value stream created by Benington and Moore (see Figure) helps us examine all the above factors via the various stages of a system (inputs, activities, co-production, outputs, user satisfaction and outcomes). It enables decision-makers to assess at each stage whether public value is added, subtracted, or stagnant, thus giving the opportunity for corrective action to be taken in order to increase public value or at least not to minimize it.
Inputs. Recruiting the right staff, obtaining resources from reputable sources, availability of appropriate technology ensures organizational capability and helps organization in creating public value.
Activities. Public value can also be reflected in the organization’s activities such as transparent decision-making, explicit criteria for priority setting, inclusive and equitable policies, and evidence-based clinical practice.
Co-production. Inclusion of patients, families and communities in their care is public value. Collaboration between organizations (for example: integration between primary and secondary care organizations) increases public value and adds value to the healthcare system.
Outputs. Ensuring organization’s efficiency through increasing production (number of interventions) and minimizing waste (money or time) while maintaining quality adds public value.
User satisfaction. Concentrating on user needs during care and ensuring a positive experience increases public value and adds value to healthcare organizations through improved reputation.
Outcomes. Preventing illnesses, improving health conditions of community members, and lowering the financial burden of illness are examples of ultimate public value.
Reading Material
-
- Moore M. Creating public value. Harvard University Press. 1995.
- Moore M and Benington J. Public value. Theory and practice. Palgrave Macmillan. 2011.
- Hartley J and Benington J. Leadership for healthcare. The Policy Press. 2010.
- Leonard H. A short note on public sector strategy-building. Harvard University. 2002.
- Williams I and Shearer H. Public value and the English NHS. A review of literature. NHS. 2010.
- Kelly G, Mulgan G, Muers S. Creating public value. An analytical framework for public service reform. Cabinet Office, UK. 2002.